Telephone
888-LAB-8082 (888-522-8082)
Email Address
info@empirecitylabs.com
Corporate Headquarters
229 49th St Brooklyn NY 11220
888-LAB-8082 (888-522-8082)
info@empirecitylabs.com
229 49th St Brooklyn NY 11220
AutoCyte prep system utilizes a liquid- based thin-layer cell preparation process. The intention behind this procedure is to generate; slides that substitute conventional gynecological pap smears. The purpose of these slides are
used to screen for and detect cervical / vaginal conditions such as cervical cancer, pre-cancerous lesions, atypical cells and others defined by the Bethesda system for reporting Cervical/ Vaginal cytologic diagnoses. Collection of AutoCyte
PREP (SurePath Thin layer cervical sample); method is as follows:
1. Take the Rover cervex-brush and insert into the endo-cervical canal.
2. Gently apply pressure against the cervix until bristles form.
3. Hold the stem between the thumb and forefinger, rotate the brush 5 times in a clockwise direction WHILE maintaining gentle pressure.
4. Remove the cervex-brush.
5. Disconnect the entire brush from the stem by pressing your thumb against the back of the brush and proceed to drop it into the preservative vial.
6. Be sure to place the vial cap on and tighten.
7. Properly label the vial using the patients full name, ID number and or physician name/ date if required.
8. Complete the requisition form with the appropriate data.
9. Place the vial and matching requisition into a specimen bag and send off to Cytopathology lab.
10. All supplies are intended for single use ONLY
WARNINGS:
CytoRich preservative fluid consists of a denatured and dilute solution of ethanol NOT intended for human consumption. The mixture includes minor amounts of methanol and isopropanol which may cause blindness and be harmful if ingested
CytoRich reagent also consists of Sodium azide. Proper care should be taken upon disposal by flushing with a large amount of water to prevent a buildup of azide.
1. 9:1 blood to anticoagulant ratio is needed. Routine collection yields 4.5 mL blood added to 0.5 mL sodium citrate. The vacutainer tube must be completely full.
2. 3.2% Sodium citrate plasma frozen is the only sample type for coagulation testing. Any other anticoagulants (heparin, EDTA, oxalate) CANNOT be accepted.
**Note:For patients with normal hematocrits, no anticoagulant adjustment is needed. If the patient has an
elevated hematocrit the level of anticoagulant in the tube must be adjusted.High hematocrit patients will have less plasma with an increased concentration of sodium citrate. The test result will be falsely prolonged in a patient
with a hematocrit of 55% or greater. The amount of sodium citrate should be adjusted using the following formula:
3. To avoid contaminating samples with tissue thromboplastin or heparin, follow the guidelines below. These substances incur a possibility of altering results.
– The venipuncture must be clean.
– The first 5.0 mL of blood drawn from a patient should not be used for coagulation testing, unless using a vacutainer/needle assembly for Protime and PTT draw.
– Hemolyzed samples cannot be utilized
– The first 15 mL of blood drawn from an indwelling catheter must be discarded or used for other lab tests before the specimen for coagulation testing can be acquired.
4. Mix the sample gently by inverting the tube several times immediately after filling. Do not shake the tube as this will break down fibrinogen in the sample. After adjusting the anticoagulant, the blood must be drawn in a syringe and the tubes filled
from the syringe as the vacuum has been removed from the tube.
Procedure for Preparing Platelet-Poor Plasma
Follow steps 1-4 of General Drawing Instructions.
5. Less platelets present in the specimen, the greater the accuracy of results will be.
6. It is considered to be more ideal that platelet-poor plasma (PPP) should have a platelet count of less than 10 x 109per liter. It is considered vital for laboratories to perform double centrifugation in order to achieve an
optimal PPP. The double centrifuge technique is:
-Within 30 minutes of draw time- Spin down specimen at 3000 RPM (1600 g) for a total of 10 minutes.
– Transfer the plasma to a plastic tube with a plastic Pasteur pipet,, avoid the buffy coat layer. Glass Pasteur pipets or glass tubes are not acceptable as glass can activate the clotting cascade.
– Once more, spin down the plasma portion again at 3000 RPM for 10 minutes. Using another plastic Pasteur pipet, move the plasma to another plastic tube, staying clear of the bottom of the tube where the platelets lie. This will not only
give platelet-poor plasma, but present a sample that is as platelet poor as possible. It is substantial to remove as many platelets as possible, as any residual platelets will lyse due to the freezing process required for shipping.
7. Transfer plasma to a plastic tube and quick freeze the sample. Ship specimen on dry ice and ensure it remains frozen for the remainder of the time it is in transit.
Specimen collection instruction:
1. One specimen per day should be collected unless otherwise instructed.
2. Avoid contamination with urine. Stool should be passed directly into the specimen container or a large clean container.
3. Label the container with the appropriate fields (name, date, time of collection)
4. Specimen must be submitted to lab within 2 hours of collection.
Requirement and procedures to handle specimens that CANNOT be transported to a laboratory facility within 2 hours:
Stool for WBC: TRANSPORT MEDIA IS UNAVAILABLE FOR THIS TEST. Specimen submitted within a 24hr time span is crucial.
Clostridium Difficile: Within 24hrs, refrigerate and submit specimen
Ova and parasites: Vials should remain at room temperature and submitted within a 24hr period. Label each container (with your name, time of collection, date, and mark the block for specimen appearance). Add stool into the vials
of transport media until the fluid level rises to the black arrow.
Culture for pathogens: Add stool into the vials until fluid level rises to the red line. Place cap and mix gently. Label the container (your name, time of collection, date, and if the specimen is bloody, write the word bloody
on the container as an indicator of this.
Occult Blood: Within 24hrs, refrigerate and submit stool to the laboratory.
False positive results could occur from:
Antacids (Rolaid, Tums, Peptobismol)
Vitamin C
False positive results could occur from:
Aspirin and alcohol
Fruits and vegetables that are rich in peroxidase.
Red meat
Iron
Gastric irritants
| SPECIMEN | FLOW | PCR | RT_PCR | CYTOGENETICS CHROMOSOME FISH | SHIPPING |
|---|---|---|---|---|---|
Peripheral Blood | Green, yellow or lavender-top tube and 1 smear | Lavender-top tube 5mL | Lavender-top tube 6mL | Green-top tube 2-5mL | Within 48hrs Room temperature |
Fresh bone marrow core biopsy | RPMI Media 1cm with no fixative | 1cm RPMI Media | N/A | 1cm RPMI Media No fixative | Within 48hrs Room temperature |
Bone marrow aspirate | Green-top tube 2mL 1 Fresh smear | Lavender-top tube 2-5mL | Lavender-top tube 2-5mL | Green-top tube 2-5mL | Within 48hrs Room temperature |
Fresh tissue biopsy | RPMI Media 1cm For optimal cell preservation, dice into fine pieces. | 10% Formalin divides into sections no bigger than 0.5% | N/A | RPMI MEDIA 1cm | Within 48hrs Room temperature |
Frozen tissue biopsy | N/A | Snap frozen | .5 x .5 x .5 (B5 is unacceptable) | N/A | Dry ice |
Fixed paraffin | N/A | .5 x .5 x .5 (B5 is unacceptable | N/A | Call the lab | Room temperature |
A FEW THINGS TO CONSIDER:
Whenever possible, specimens should be attained before any antimicrobial agents or antibiotics have been administered.
Clinical specimens should be collected in leak-proof specimen containers that are tightly sealed.
Material should be collected where the suspected organism is most likely to be locateed and with the least amount of external contamination as possible
The stage of the disease is at times a vital regard in the successful isolation of the causative agent.
Specimens quantity should suffice to permit completion of all tests ordered.
Provisions should be made for the prompt delivery (within one hour after collection)
In most cases, clinical specimens can be refrigerated allowing them to be held for a number of hours before beginning to culture. DO NOT refrigerate any bodily fluids.
Specimens for Neisseria gonorrhoeae isolation MUST be submitted on appropriate isolation plates. Inoculated plates cannot be refrigerated.
Ova and parasite exams ALL require formalin fixative preservation and PVA or equilavent.
PVA fixatives are required for all soft and liquid stools to maintain the integrity of the trophozoites in the trichrome stain.
Collect watery, loose, or unformed stools and submit promptly to the laboratory for
Clostridium difficile PCR testing for hospitalized patients. Repeat testing appears rarely useful, except for patients with evidence of a new infection.
It is suggested to collect three (3) sputum specimens for acid-fast smears and culture in patients with clinical and chest x-ray findings compatible with tuberculosis for mycobacterial (TB) culture. These three (3) samples should be collected at 8-24
hour intervals (24 hours when possible) and should include at least one first morning specimen.
RECOMMENDATIONS FOR COLLECTING BLOOD CULTURES
1. For each septic episode, draw 2 to 3 separate sets within a 24-hour period, spaced as far apart as possible (a minimum of 30 minutes between sets).
2. For initial cultures: Suspected sepsis: 2 separate sets before antimicrobial therapy is started; spaced a minimum of 30 minutes apart.
3. Wait at least 72 hours from the time of first set for identification and sensitivity results before obtaining additional cultures.
4. Draw a maximum of 3 more blood cultures over the course of 24 hours If cultures are still negative after 72 hours and the clinical condition warrants it. Wait another 72 hours for results.
SPECIMEN COLLECTION AND HANDLING
BLOOD CULTURE COLLECTION PROCEDURE
Materials Required:
· 1-2% tincture of iodine or 2% chlorhexidine
1. Locate vein for venipuncture site and put on gloves.
2. Using an alcohol prep, vigorously cleanse the intended venipuncture site for 30 seconds back and forth followed by tincture of iodine which is allowed to dry for at least 30 seconds or 2% chlorhexidine, to dry for at least 30 seconds to allow time
for the micro organisms on the skin’s surface to die.
3. Remove the caps from one aerobic blood culture bottle and one anaerobic blood culture bottle. Clean each rubber septum with an alcohol prep.
4. Prep the syringe and execute the venipuncture. A smaller draw volume,1-3 mL, is enough for pediatric patients. Pediatric blood culture bottles are available to use.
VIRAL AND CHLAMYDIAL TESTS
Viral and Chlamydial Cultures:
· Viral Chlamydial Transport Medium (VCM). IMPORTANT: After sample collection, specimen cultures should be refrigerated until pick up.
GEN-PROBE® PACE® 2 Collection Kit (male or female); stable at ambient temperatures until printed expiration date.
COLLECTION FROM NORMALLY STERILE SITES AEROBIC CULTURE
Decontaminate site by cleaning puncture site with a povidone-iodine preparations or similar disinfectant to remain on skin for atleast one minute
Proceed to use a 70% alcohol swab to clean the intended site of puncture.
BLOOD COLLECTION (USED FOR BRUCELLA CULTURE)
Blood bottles must be submitted. Decontaminate by swabbing with iodine proceeding with alcohol to remove iodine.
After blood specimen collection, inject 10mL into each of the 2 bottles, and swirl to mix. Store at room temperature until sent to lab.
CEREBROSPINAL FLUID
For each test ordered, submit sterile, screw-capped tubes with .75mL (at minimum) for each test.
OTHER STERILE BODY FLUID
Specimens may be submitted in sterile containers for aerobic culture only.
Follow standard procedures and obtain the specimen by aspiration. Transport the specimen in aerobic or anaerobic transport kits or blood culture bottles.
COLLECTION FROM NONSTERILE SITE
SPUTUM SPECIMENS
collection in the early morning is recommended for routine sputum specimens. Patient should gargle with water before collection. The most preferred specimen is that of the expectoration obtained after a deep cough. Specimen should be in a leak-proof plastic
container.
URINE SPECIMENS
All patients should void the first part of the specimen into the toilet, then collect the remainder of the specimen in a sterile container. Urine samples for mycobacteria or fungus culture may be submitted in a sterile screw cap container. Keep urine
refrigerated.
In order to accquire a clean catch sample of urine from a female patient, a thorough cleansing of the periurethral area is crucial before specimen collection. Wash the area with a disinfectant, thoroughly rinse with clean water, and make all efforts to
avoid any contact until urination is complete.
For a male patient, a thorough cleansing of the glans penis with disinfectant followed by a complete rinse with clean water is required as well
For in-dwelling catheters, obtain the specimen with a needle and syringe. Select a puncture site 1-2 inches distal to the meatus and clamp below the puncture site. Cleanse the area to be punctured with 70% alcohol. Aspirate exactly 5 mL of urine with
a sterile needle and syringe. Specimens obtained from the collection bag are not suitable for analysis.
For cytoscopic or suprapubic aspiration, follow standard procedure and obtain the specimen by aspiration. Transport the specimen in anaerobic transport tubes. Keep urine refrigerated.
STOOL CULTURE
Stool should be collected without contamination from urine . Select portions of stool (containing pus, blood or mucus) and immediately mix into modified Cary-Blair transport media otherwise they will NOT be accepted (frozen specimens will also not be
accepted).
ANAEROBIC CULTURE
Specimens from the following sites are acceptable when submitted in appropriate transport:
Transtracheal aspirations
Suprapubic urines from percutaneous suprapubic bladder, nephrostomy tube or suprapubic catheter
Genital specimens from cul-de-sac aspiration, culdocentesis, percutaneous aspiration, placenta, fallopian tube, or prostatic or seminal fluid
Surgical specimens
Exudates, aspirated pus from deep wounds or abscesses
Body fluids – normally sterile
Specimens from the following sites are not acceptable:
Throat and nasopharyngeal swabs
Sputum and bronchoscopy specimens
Feces and rectal swabs except for C. difficile Cultures
Voided or catheterized urines
Specimens from sites contaminated with intestinal contents such as colostomy sites, draining pilonidal sinus and traumatic perforation of the bowel
Superficial wounds
Vaginal or cervical swabs
BRONCHIAL WASH
3mL of Bronchial washings into a sterile container or a sterile container with sterile saline ONLY.
CSF
Collect 1 mL CSF (minimum) in a sterile plastic conical tube, tightly sealed.
GASTRIC
Any gastric samples are unaccceptable unless they have been adjusted to a neutral PH.Use a sterile saline and collect an early morning specimen (fasting required)
SPUTUM
Sputum should be collected using a sputum collection kit. A 5-10mL of first morning sputum is preferred. Salive as well as specimens in 70% alcohol won’t be accepted.
URINE
Collect up to 50 mL of first morning urine specimen. Send in a tightly sealed sterile plastic container.
BONE MARROW
Collect as much as possible into an SPS or heparin blood collection tube.
BODY FLUIDS
Present at least 10-15 mL in a leakproof sterile container. Collect bloody specimens into a SPS blood collection tube (yellow-top).
TISSUE BIOPSY SAMPLE
In a sterile container without fixative or preservative submit I gram of tissue. Keep moist with a small quantity of sterile saline or nutritive broth. Collect aseptically and avoid indigenous microbiota. Select caseous portion if available. Refrigerating
is ok however, DO NOT freeze.
LYMPH NODE
Submit a sample of a node in a sterile container without fixative or preservative. Collect aseptically and avoid indigenous microbiota. Refrigeration is acceptable. Do not freeze
SKIN LESION MATERIAL
Submit biopsy specimen in sterile container without fixative or preservative. Swabs in transport medium are acceptable only if biopsy sample material or aspirate is not obtainable. For a cutaneous ulcer, collect the biopsy sample from the periphery of
the lesion, or aspirate material from under the margin of the lesion.
CULTURE FOR FUNGI
Collect specimens from the following sites using a culture swab transport medium system: mouth, nose, nasopharynx, ear, eye, wound, vagina, cervix, or urethra. Use a sterile plastic container for respiratory secretions, body fluids, tissue, bone marrow,
CSF, urine, hair, skin, nail, contact lens fluid and/or contact lenses. Refer to the database for the current collection method for blood. Store and transport specimens at 4°C. Dermatological specimens may be shipped at 15-30°C.
MYCOPLASMA/UREAPLASMA CULTURES
General considerations: All specimens must be transported in the multi-microbe transport media (VCM supplied at your request). Samples submitted without suitable transport media will not be accepted. Refrigerated stability for all mycoplasma/ureaplasma
cultures is 48 hours. Specimens transported and stored at -70°C are stable indefinitely. Freezing is preferred if transport time is expected to exceed 24 hours. It is preferable to vigorously agitate the swab in the transport media for 30
seconds, and express the material from the swab into the transport media. Discard the swab. Inhibitory agents may be present in the material of the swab tip or shaft. If viral cultures are requested, submit a separate sample according to the
standards outlined in the virology section.
MYCOPLASMA PNEUMONIAE
Collect tracheal aspirate, sputum, throat or nasopharyngeal swabs and submit in the multi-microbe transport medium (VCM) supplied upon request. Refrigerate(48-hr stability) or freeze at -70°C (indefinite stability; transport on dry ice: do not thaw).
Freezing is preferred if transport time is expected to exceed 24 hours.
UREAPLASMA UREALYTICUM AND M. HOMINIS
Collect tracheal aspirates from newborns to detect pneumonia caused by ureaplasma urealyticum Submit in multi-microbe transport medium (VCM) supplied upon request. Refrigerate (48-hr stability) or freeze at -70°C (indefinite stability; transport on dry
ice; do not thaw). Freezing is preferred if transport time is expected to exceed 24 hours. Adult genital specimens include: vaginal, cervical or urethral swabs, amniotic fluid, CSF, urine or semen submitted in multi-microbe transport refrigerated
or frozen as detailed above.
NUCLEIC ACID TESTS (BDNA, PCR, TMA, GENOTYPING, ETC.)
Standard quantitative assay: 1 mL frozen PPT-potassium EDTA plasma (white-top tube); (bDNA, PCR, TMA, Genotyping, etc.) 0.5 mL minimum
Ultrasensitive assay
: 2.0 mL frozen PPT-potassium EDTA plasma (white-top tube); 0.6 mL minimum
Expanded range assay
: 2.5 mL frozen PPT-potassium EDTA plasma (white-top tube); 1.0 mL minimum
Centrifuge blood within 2 hours of collection and freeze without removing the plasma without thawing OR submit EDTA (lavender-top tube) or ACD (yellow-top tube) frozen plasma that has been removed from cells and frozen within 2 hours of collection. Repeated
freezing and thawing is not recommended.
**Note that specimens collected in ACD anticoagulant will have results that are 15% lower than those collected in EDTA.
PARASITOLOGY
OVA AND PARASITE STUDIES
Three specimens on separate days within a 10 day period is recommended. Stool should be collected without contamination by urine. Within an hour (maximum) stool should be mixed into both a modified PVA and 1-% formalin containers. Specimens should be
stored at room temperature. Specimens without preservatives will not be accepted.
MALARIA/BLOOD PARASITE STUDIES
Smears should be prepared within a 24hr range after specimen collection. Thin and thick smears should be presented in a slide carrier. Each sample should include of EDTA whole blood. Slides should be air dried ONLY.
MISCELLANEOUS
CLOSTRIDIUM DIFFICILE TOXIN, EIA OR TISSUE CULTURE, STOOL
Fresh stool in a sterile, leak-proof container (without metal ions, serum, preservatives, media or additives). If transport time is to exceed 24 hours, specimen should be frozen.
| Blood culture | Broth mixture |
|---|---|
| Light blue | Sodium Citrate |
| Red | None |
| Dark green | Sodium Heparin |
| PST Light green | Lithium Heparin & gel separator |
| Red-gray or Gold SST | Gel separator & clot activator |
| Lavender | EDTA |
| Pale yellow | Acid citrate dextrose |
| Light Gray | Oxalate / Fluoride |
Bone Marrow biopsies:
5 Unstained aspirate smears along with the core biopsy and a brief summary of the differential diagnosis and clinical finds.
Results from a most recent CBC and white blood cell differential and blood smear should be submitted as well
Paraffin embedded tissues
Submit a copy of the pathology report, H&E slide correlating to the tumor block being submitted, and a formalin fixed paraffin embedded tumor tissue.
Each specimen being submitted should have a separate test request for with a notation of the fixative being used.
After testing is completed, all tumor blocks will be returned to the client.
Decalcified specimens are not recommended
Paraffin-embedded tissue fixed with formalin may be stored at room temperatures indefinately.
Paraffin Block preparation
Tissue should be trimmed free of fat and necrotic tissue. Immediately put tissue pieces in a 10 % neutral buffered formalin solution. Specimen should be fixed for a total of 4-24hrs.
Fixed tissue should be embedded into paraffin and be stored at temperatures not exceeding 60°C.
Slide Preparation
Submit 10 slides with a minimum of 5 (one 4-5 micron thick section on each slide).
Charged (+) sides must be used. All slides should be stored and shipped at ambient temperatures.
Bone Marrow, Body fluids for Leukemia/ Lumphome evaluation by cytometry, Peripheral blood, and Lymph nodes
Provide a brief clinical summary, previous diagnoses, CBC results, etc. to accompany these specimens
Collecting and shipping Peripheral blood/bone marrow for Leukemia/Lymphoma evaluation
Peripheral Blood:
5mL Whole blood in Green-top tube ( Sodium heparin) with no fixatives. Store and ship at room temperature ONLY.
Bone Marrow:
2mL Bone marrow in Green-top tube ( Sodium heparin) with no fixatives. Store and ship at room temperature ONLY.
Collecting and shipping tissue (not including bone marrow or blood) for phenotyping flow cytometry.
Any tissue(s) suspected to have a hematologic malignancy must be surgically removed and placed in a sterile, leak-proof plastic container.
Container must have a small amount of sterile RPMI-1640 tissue culture medium enough to cover the tissue (should be pink or magenta, if yellow or cloudy discard).
Tissue should not be freezed, fixed, dried out at any time.
3mL sample at minimum is needed (pea sized) is preferred.
Specimen should be stored and shipped at 4°C or room temperature.
Procedures for collecting and shipping body fluids.
Any and all body fluids should be collected and shipped in sterile, screw-cap containers.
Bloody fluids (if there are any) should be placed in Sodium heparin reen-top tubes. Samples should be stored at room temperature or 4°C.
Unless there is evident evidence of a high cell count, cerebrospinal fluid is not recomennded.
20mL of Pleural or peritoneal fluid should suffice.
PROCEDURE FOR COLLECTING AND SHIPPING SAMPLES FOR PLASMA-BASED MOLECULAR ASSAYS
Collect 5-6mL Whole blood in EDTA tubes.
Label tube with draw time and date on the tube
Ship immediately
Shipping temperature:
Whole blood
Room temp.
acceptable
: 72 hours
Refrigerated
preferred
: 72 hours
Frozen unacceptable
SPECIMEN REQUIREMENTS
For each test, the specimen type, preferred and minimum specimen volume, preferred shipping/storage temperature, and any special handling notes are specified. The preferred volume is an amount sufficient to allow multiple runs of the assay either singly
or in duplicate. The minimum volume allows one single analysis including instrument dead volume. In some situations, it may be possible to assay samples below the stated minimum volume (see below). Storage temperature is specified as room
temperature (15-30° C), refrigerated (2-10° C) or frozen (-20° C or colder). When temperature is not indicated, the sample may be stored and shipped in the most convenient manner for the client.
Precautions taken with minimum volume samples
§ Flag the tube and requisition by using red labels with the word “Pediatric”. One placed on the tube and the other in a blank field on the rest request form
§ Bring it to the attention of client services with an upfront notification. The sample could then be flagged in the system and be handled with special attention. The ordering physician could also list the priority of testing ahead of time on the requisition
form.
**Note, in some situations, it may be permitted to perform an assay on a sample whose volume is less than the stated minimum (typically by performing the test on a diluted sample, if the assay and the clinical situation permit). Please call Client Services
to arrange for consultation.
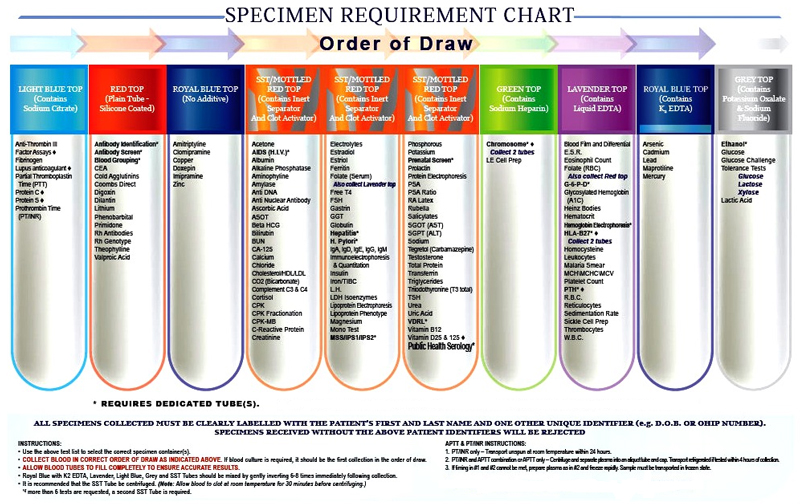
SPECIMEN COLLECTION: SERUM, PLASMA, OR BLOOD
Blood should be drawn in the color coded tube indicated on the test requirement.
It is recommended to draw 2.5 times the requested volume for both serum and plasma
Blood should be allowed to clot for at least 10minutes and centrifuged for any draws involving the use of serum
Plasma and whole blood the tube should be filled completely to eliminate dilution from any anticoagulant or preservative. It should immediately mixed by inverting the tube anywhere from 5-10 times.
Plasma should also be separated by centrifugation.
Once the steps previously mentioned have been taken, transfer the specimen to a plastic transport tube.
SPECIMEN COLLECTION: URINE
Any medications the patient has taken should be documented and recorded.
If there are any preservatives or additives required, the designated additive should be in the in the container at the beginning of the collection.
Patients should be pre-cautioned that the added preservative should not be discarded or spilled and may be toxic.
First morning void urine should be discarded, following this collection should begin. Morning urine void on the 2nd day should be considered the final collection
Total collection of 24hr urine volume should be measured. Document measured volume on the requisition form and urine transport container. Then transfer the requested volume into the labeled transport vial.
Do not send the entire urine collection.
SHIPPING TEMPERATURE
Each tube or container should be labeled as follows:
Patient Name
Patient Date of Birth*
Client Name
Client/Patient #
Date of Collection
Time of Collection
Test Codes Ordered
FURTHERMORE
Standard tubes should have the labels affixed lengthwise down the tube.
Indicate patient’s age so appropriate reference ranges can be administered.
Most acute infections elicit a predictable immune response. There are some important exceptions, however:
Despite significant illness, some superficial infections could fail to induce an antibody response.
Immunocompromised individuals may not produce any significant antibody response either despite infection.
The presence of IGM antibodies precede the appearance of IGG antibodies. IGM antibodies are also an indicator of recent or current exposure to infection, not necessarily primary infection. IGM antibodies typically appear 7-10 Days after a primary infection
and reaches peak levels within 2-3 weeks.
The presence of IGG is an indicator of immunization, past exposure or infection to the organism. This also suggests immunity to rubella or measles. Antibody/serology tests are designed to detect multiple or specific classes of immunoglobulins (e.g., total
antibody vs. specific IgG or IgM).
SPECIMEN COLLECTION AND HANDLING
Serum:
Collect blood in a red-top or serum separate tube (SST).
Cerebrospinal Fluid (CSF):
CSF will be accepted only for serologic testing for certain organisms that are associated with neurological diseases.. Collect blood-free CSF as directed in the Specimen Collection and Handling section of this directory. Refrigerate at 4°C until transported
to the lab. There may need to collect a serum sample at the same time for serologic diagnosis of central nervous system diseases.
Other Body Fluids:
Fluids other than serum and CSF are not acceptable.
Serum:
Blood should be collected in a plain red-top tube. Gel barrier tubes are not acceptable. Blood should be sustained at room temperature and let to clot for 20-30 minutes. Centrifuge at 800-1000g for 10-15min. Transport serum into polyethylene or polypropylene
transport tube.
Plasma:
In an EDTA Lavender-top tube, collect specimen. Let red cells settle. Transfer into a polyethylene transport tube. Transport in the appropriate temperature.
Determining trace elements:
Serum:
Patients should avoid taking any vitamins, mineral supplements or antacids for at least 3 days prior to specimen collection.
Specimens should be alotted 30min to clot at room temperature. Centrifuge at 800-1000g for 10-15min. Pour serum into trace element plastic shipping container.
Use Royal blue-top tubes for specimen collection (tubes certified free of the trace element being tested).
Specimens should be shipped refrigerated.
Plasma:
Royal blue-top tubes should be utilized in order to perform the assay. Be sure the vial is certified free of the trace element in question.
Mix the specimen gently and centrifuge.
Pour the specimen into a plastic shipping container designated for trace element testing.
Patients should avoid taking any vitamins, mineral supplements, or antacids prior to specimen collection.
Whole blood:
Patients should avoid taking any vitamins, mineral supplements or antacids for at least 3 days prior to specimen collection.
Specimen should be collected in tubes Royal blue-top tubes containing EDTA voided of any trace elements being tested for.
Specimen should be gently mixed right after collection.
Protect specimen from light by wrapping tube in aluminum foil.
Urine:
Urine should be collected in a clean or acid washed container voided of any trace elements.
Patients should avoid taking any vitamins, mineral supplements, seafood or antacids for at least 3 days prior to specimen collection.
Be sure to reduce the risk of contamination by washing hands prior to each time opening the container.
After urine is mixed well, carefully pour contents into an acid washed container (random urine, if possible should have 2 aliquots prepared).
Urine used for trace element assays if not sent within 24hrs should be shipped and stored frozen.
Make a notation of urine type on the requisition form.
General Precautions
Specimens are subject to rejection if specimens are submitted with :
Gel based swabs
Within insufficient volumes
Leakage
Sent with needles
Sent with bacteria culture bottles or BacTec
Diapers
Non MCV or equivalent
Specimen Handling
Specimen should be collected within a few days on the onset of clinical symptoms from the associated site.
Use an aseptical method to collect specimen
Do not freeze specimen unless specifically stated otherwise. Viruses can only be frozen if submitted in a VCM or equivalent and have a maximum stability of 3 days.
Do not use wooden swabs
Use the appropriate specimen collection kit
Chlamydia Culture
Swab
Use a sterile swab to remove mucous and sterile dacron swabs to attain columnar/cuboidal epithelial cells. Wooden or cotton swabs are
unacceptable. Use a VCM or equivalent. Specimens may be kept frozen at -70°C for up to 5 days.
Urine
Use nucleic acid amplification methodologies such as PCR or TMA. Culture methodology is
Test slide
Use a specimen collection kit. Specimen should be stored at room temperature pr refrigerated with stability up to a week
Chlamydia Probe (GenProbe)
Swab only
GenProbe specimen collection kits should be used for Urethral, conjunctival, or cervical specimens. Specimens have a stability up to a week and cannot be frozen.
Viral DFA
Slide
Collect cellular material using a sterile swab. Transfer specimen using a cytospin preparation or clean glass slide. Specimen is stable up tp a week stored at room temperature
Specimen should be collected aseptically and should utilize a VCM or equivalent. Refrigerate.
Viral cultures
It is recommended that specimens be refrigerated and shipped as soon as possible. Unless specimen is in a VCM or equivalent do not freeze varicella, RSV, measles or CMV specimens. Bone marrow and whole blood cannot utilize a VCM or be frozen
.
Autopsy/ Biopsy Tissue
For each specimen needed, use a sterile set of instruments and place into separate tubes of VCM (or equivalent) with no added fixatives.
Specimens in VCM are stable for up to 5 days frozen at -70°.
Bone marrow
0.3mL of aspirate or 1.5 x 0.3cm size biopsy and transport specimen into a VCM.
Blood
Collect 7.5-10mL Whole blood in sodium heparin tube. Specimen cannot be frozen.
Cervix
Use a VCM (or equivalent) container and a sterile swab to collect mucous.
Broncoalveolar Lavage
Insert bronchoscope into subsegmental bronchus and proceed to insert four 50mL doses of sterile saline into the suction port, immediately after the insertion of each sample return suction.
Give in 5-10mL in a sterile container.
Conjunctiva
VCM (or equivalent) container should be used for transport.
Remove any exudate or mucous using a sterile swab. Discard after.
Pre-moisten a sterile swab using sterile saline. Continue to firmly rub over the palpebral conjunctiva.
Cerebrospinal Fluid
Submit 1-2mL CSF fluiod in a sterile, leakproof polypropylene container collected aseptically.
Endourethral swab
Use a small wire-shafted dacron swab and insert 2-4cm into the edourethra.
Rotate the swab gently and then wait a few seconds.
Withdraw and put the swab into the VCM (blue or red cap), break and be sure to seal tightly.
Endocervical Swab
Use a cleansing swab to remove any mucous or exudate from the endocervix
.
Place swab into the endocervix, rotate, and remove.
Insert another swab into the cervical os to collect from the transitional zone.
Using firm contact with endocervical surfaces, rotate swab for 10-30 seconds. Place the swab into the VCM without touching any vaginal surfaces.
Fluids
Collect specimen using an aseptical method and submit within an equal porpotion to VCM
Nasal wash
Using a sterile disposable ear syringe bulb with 3-5mL of sterile saline.
Have the patient tilt their head back and insert the tip of the syringe bulb in the lower nostril.
Instill the saline into each nostril and collect into a sterile container as the patient put their head forward.
Lesion
Cut open the lesion and using a sterile swabs, collect the fluids and cells from the base of it. Use a VCM or anything equivalent.
Specimens are stable up to 5 days frozen temperatures of 70°C
Nasopharyngeal
Use a sterile flexible fine-shafted swab to insert into the nostril into the posterior nasopharynx and rotate gently
Use another sterile swab for the other nostril/
Transport both into the same VCM container ( or equivalent). The same can be done for throat swabs.
Specimens are stable up to 5 days frozen temperatures of 70°C
Rectal swab
Use a dacron swab and insert into the anal orifice about 3-5cm. Rotate the swab, withdraw and place it into a VCM
Sputum
In response to a deep cough, collect expectorate and transport in a sterile container.
Stool
Collect specimen in a clean dry container voided of any fixatives or preservatives.
Submit into a stool container.
Specimens are stable up to 5 days frozen temperatures of 70°C
Urine
Collect 2-10mL of clean catch urine submitted in a sterile, leak-proof container.
Freezing is unacceptable unless VCM or equivalent is used
Vesicle
Initially rupture the vesicle.
Rub the fluid and cells from the bottom of the vesicle using a dacron swab.
Submit the swab in a VCM and seal tightly.
After specimen has been collected, use a local disinfectant.
© 2008-2021 Empire City Laboratories, Inc. All Rights Reserved. ECL and Empire City Laboratories are registered trademarks of Empire City Laboratories®, Inc.